Cholesterol
Highlights
Total Cholesterol Goals
A blood test is used to measure cholesterol levels. A person’s total cholesterol level is determined from calculations and measurements of low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides. Standard total cholesterol goals for adults are:
- Less than 200 mg/dL is desirable
- Between 200 - 239 mg/dL is considered borderline
- Over 240 mg/dL is considered high
Lifestyle Changes
The first step to improving cholesterol levels is through lifestyle changes (especially diet and exercise). Even when drug therapy is required, lifestyle changes are also necessary. These include:
- Eat a heart-healthy diet with plenty of fiber-rich fruits and vegetables. Avoid saturated fats (found mostly in animal products) and trans-fatty acids (found in fast foods and commercially baked products). Instead, choose unsaturated fats (particularly omega-3 fatty acids found in fish oils and olive and canola oils).
- Avoid added sugars such as those found in sugar-sweetened beverages.
- Exercise regularly. Regular aerobic exercise can help boost HDL (“good” cholesterol) levels and reduce unhealthy triglycerides.
- Quit smoking.
- Try to maintain a healthy weight.
Triglycerides and Heart Health
The American Heart Association’s 2011 scientific statement on triglycerides and heart health recommends an optimal triglyceride level of below 100 mg/dL (below 150 mg/dL is considered normal). Triglycerides are unhealthy blood fats that can be significantly reduced by weight control, dietary changes, avoiding alcohol, and regular exercise. Lifestyle changes – not drugs – are the best ways to improve your triglyceride levels.
Drug Warnings and Concerns
- In 2012, the Food and Drug Administration (FDA) updated the prescribing labels of all statin drugs to include additional safety information The new labels now warn that statins may slightly increase the risk of high blood sugar and type 2 diabetes. Statins may also cause certain mental changes such as memory loss and confusion. These symptoms almost always resolve once the drug is stopped. Discuss any concerns with your doctor.
- In 2011, the FDA warned that fenofibric acid (Trilipix) may not help prevent heart attacks or strokes. Other studies have questioned the value of fibrate drugs in cholesterol treatment and raised concerns about side effects. These drugs are sometimes prescribed to patients with diabetes to help boost HDL levels.
- In 2011, the National Institutes of Health halted a clinical trial on combination statin and high-dose niacin drug therapy. This study found that the combination of drugs did not provide benefits over and above the benefits of a statin alone.
Drug Approvals
- Atorvastatin (Lipitor) is now available as a generic.
- Juvisync is a new two-in-one pill that combines the statin drug simvastatin (Zocor, generic) with the type 2 diabetes drug sitagliptin (Januvia).
Introduction
Lipids are the building blocks of the fats and fatty substances found in animals and plants. They are microscopic layered spheres of oil, which, in animals, are composed mainly of cholesterol, triglycerides, proteins (called lipoproteins), and phospholipids (molecules made up of phosphoric acid, fatty acids, and nitrogen). Lipids do not dissolve in water and are stored in the body to serve as sources of energy.
Cholesterol
Cholesterol is present in all animal cells and in animal-based foods (not in plants). In spite of its bad press, cholesterol is an essential nutrient necessary for many functions, including:
- Repairing cell membranes
- Manufacturing vitamin D in the skin
- Producing hormones, such as estrogen and testosterone
- Possibly helping cell connections in the brain that are important for learning and memory
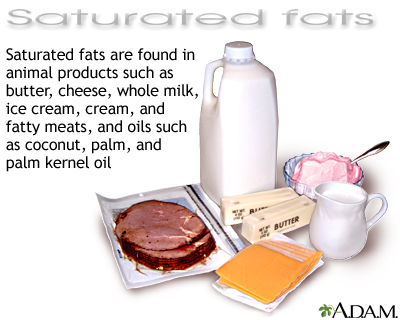
Regardless of these benefits, when cholesterol levels rise in the blood, they can have dangerous consequences, depending on the type of cholesterol. Although the body acquires some cholesterol through diet, about two-thirds is manufactured in the liver, its production stimulated by saturated fat. Saturated fats are found in animal products (meat, egg yolks, high-fat dairy products) and tropical plant oils (palm, coconut).
Triglycerides
Triglycerides are composed of fatty acid molecules. They are the basic chemicals contained in fats in both animals and plants. High levels of triglycerides, especially in combination with low levels of HDL, are associated with increased risk for heart disease, stroke, diabetes, and fatty liver disease
Lipoproteins
Lipoproteins are protein spheres that transport cholesterol, triglyceride, or other lipid molecules through the bloodstream. Most of the vascular effects of cholesterol and triglyceride actually depend on lipoproteins.
Lipoproteins are categorized into five types according to size and density. They can be further defined by whether they carry cholesterol or triglycerides.
Cholesterol-Carrying Lipoproteins. These are the lipoproteins commonly referred to as cholesterol.
- Low density lipoproteins (LDL). (Often called "bad" cholesterol.)
- High-density lipoproteins (HDL), the smallest and most dense. (Often called "good" cholesterol.)
Triglyceride-Carrying Lipoproteins.
- Intermediate density lipoproteins (IDL). They tend to carry triglycerides.
- Very low density lipoproteins (VLDL). These tend to carry triglycerides.
- Chylomicrons (largest in size and lowest in density).
Effects of Lipoproteins and Triglycerides on Heart Disease
Low Density Lipoproteins (LDL), the "Bad"Cholesterol. The main villain in the cholesterol story is low-density lipoprotein (LDL). Heart disease is least likely to occur among people with the lowest LDL levels. Lowering LDL is the primary goal of cholesterol drug and lifestyle therapy.
Low-density lipoprotein (LDL) transports about 75% of the blood's cholesterol to the body's cells. It is normally harmless. However, if it is exposed to a process called oxidation, LDL can penetrate and interact dangerously with the walls of the artery, producing a harmful inflammatory response. Oxidation is a natural process in the body that occurs from chemical combinations with unstable molecules. These molecules are known as oxygen-free radicals or oxidants.
In response to oxidized LDL, the body releases various immune factors aimed at protecting the damaged arterial walls. Unfortunately, in excessive quantities they cause inflammation and promote further injury to the areas they target.
High Density Lipoproteins (HDL), the "Good" Cholesterol. High density lipoprotein (HDL) appears to benefit the body in two ways:
- It removes cholesterol from the walls of the arteries and returns it to the liver for disposal from the body.
- It helps prevent oxidation of LDL. HDL actually appears to have its own antioxidant properties.
- It may also fight inflammation.
HDL helps keep arteries open and reduces the risk for heart attack. High levels of HDL (above 60 mg/dL) may be nearly as protective for the heart as low levels of LDL. HDL levels below 40 mg/dL are associated with an increased risk of heart disease.
Triglycerides. Triglycerides interact with HDL cholesterol in such a way that HDL levels fall as triglyceride levels rise. High triglycerides may pose other dangers, regardless of cholesterol levels. For example, they may be associated with blood clots that form and block the arteries. High triglyceride levels are also associated with the inflammatory response -- the harmful effect of an overactive immune system that can cause considerable damage to cells and tissues, including the arteries.
Cholesterol and Triglycerides Goals
Total cholesterol count includes measurements of LDL, HDL, and triglycerides. The following chart summarizes all lipid goals for adults.
Cholesterol Goals for Adults | |||
Total Cholesterol Goals | LDL Goals | HDL Goals | Triglyceride Goals |
Less than 200 mg/dL is desirable. Between 200 and 239 is borderline. Over 240 is high. | 70 mg/dL is considered an important goal for very high-risk patients (recent heart attack; current active or unstable cardiovascular or cerebrovascular disease; or two multiple risk factors as defined below.) Below 100 mg/dL is optimal for everyone. It should be the goal for high-risk people, including those with existing heart disease, diabetes, or two or more risk factors for heart disease; 70 mg/dL is an even better goal for these individuals. 130 mg/dL or below for people with two or more risk factors; 100 mg/dL is an optimal goal. 160 mg/dL or below for people at less risk (one or zero risk factors); 130 mg/dL is an optimal goal. Anything above 160mg/dL is high, with levels above 190 being very high. LDL levels over 190 often require medication even with no other cardiac risk factors present. | Levels above 40 mg/dL are desirable; levels above 60 mg/dL are optimal. | Below 150 mg/dL is normal. An optimal triglyceride level is below 100 mg/dL. 150 - 199 is borderline high. 200 - 499 is high. Over 500 is very high. |
Risk factors for heart disease include a family history of early heart problems before age 55 for men (before age 65 for women), smoking, high blood pressure, diabetes, being older (over 45 for men and 55 for women), and having HDL levels below 35 mg/dL. People with two or more of these risk factors may have a 10-year risk of heart attack that exceeds 20%, and may therefore need to aim for LDL levels of 100 mg/dL or below. | |||
Cholesterol Goals for Children. The American Heart Association’s general LDL goals for children are 190 mg/dL or less for children with no additional heart disease risk factors and 160 mg/dL or less for children with additional risk factors (such as family history of high cholesterol, heart disease, and diabetes).
Risk Factors
Unhealthy cholesterol levels (low HDL, high LDL, and high triglycerides) increase the risk for heart disease and heart attack. Some risk factors for cholesterol can be controlled (such as diet, exercise, and weight) while others cannot (such as age, gender, and family history).
Age and Gender
From puberty on, men tend to have lower HDL (“good” cholesterol) levels than women. One reason is that the female sex hormone estrogen is associated with higher HDL levels. Because of this, premenopausal women generally have lower rates of heart disease than men.
After menopause, as estrogen levels decline, women catch up in their rates of heart disease. Throughout the post-menopausal years, HDL levels decrease and LDL (“bad” cholesterol) and triglyceride levels increase. For men, LDL and triglyceride levels also rise as they age and the risks for heart disease increase as well. (There is some evidence that high triglyceride levels carry more risks for women than men.) Heart disease is the main cause of death for both men and women.
Children and Adolescents. Children who have abnormal cholesterol levels are at increased risk of developing heart disease later in life. However, it is difficult to distinguish “normal” cholesterol levels in children. Cholesterol levels tend to naturally rise sharply until puberty, decrease sharply, and then rise again.
Genetic Factors and Family History
Genetics play a major role in determining a person's blood cholesterol levels. (Children from families with a history of premature heart disease should be tested for cholesterol levels after they are 2 years old.) Genes may influence whether a person has low HDL levels, high LDL levels, high triglycerides, or high levels of other lipoproteins, such as lipoprotein(a).
Inherited cholesterol disorders include:
- Familial hypercholesterolemia is a genetic disorder that causes high cholesterol levels, particularly LDL, and premature heart disease. It occurs in as many as 1 in 500 people.
- Familial lipoprotein lipase deficiency is a very rare disorder that causes depletion of lipoprotein lipase. This is an enzyme that appears to be important in the removal of lipoproteins that are rich in triglycerides. People who are deficient in it have high levels of cholesterol and fat in their blood.
Lifestyle Factors
Diet. The primary dietary elements that lead to unhealthy blood cholesterol include saturated fats (found mainly in red meat and high-fat dairy products) and trans fatty acids (found in fried foods and some commercial baked food products). Shellfish and egg yolks are also high in dietary cholesterol. High amounts of added sugars raise triglyceride levels.
Weight. Being overweight or obese increases the risks for unhealthy cholesterol levels.
Exercise. Lack of exercise can contribute to weight gain, decreases in HDL levels, and increases in LDL, triglyercides, and total cholesterol levels.
Smoking. Smoking reduces HDL cholesterol and promotes build-up of fatty deposits in the coronary arteries.
Alcohol. Heavy consumption of alcohol can increase triglyceride levels.
Obesity, Metabolic Syndrome, and Type 2 Diabetes
In the U.S., obesity is at epidemic levels in all age groups. The effect of obesity on cholesterol levels is complex. Overweight individuals tend to have high triglyceride and LDL levels and low HDL levels. This combination is a risk factor for heart disease. Obesity also causes other effects such as high blood pressure and an increase in inflammation that pose major risks to the heart.
Obesity is particularly dangerous when it is one of the components of the metabolic syndrome. The syndrome consists of obesity marked by abdominal fat, unhealthy cholesterol levels, high blood pressure, and insulin resistance. Metabolic syndrome is a pre-diabetic condition that is significantly associated with heart disease and higher mortality rates from all causes. Obesity is also strongly associated with type 2 diabetes, which itself poses a significant risk for high cholesterol levels and heart disease.
Children who are overweight are at higher risk for high triglycerides and low HDL, which may be directly related to later unhealthy cholesterol levels. Childhood LDL levels and body mass index (BMI) are strongly associated with cardiovascular risk during adulthood. Overweight and obese children who have high cholesterol should also get tested for high blood pressure, diabetes, and other conditions associated with metabolic syndrome.
Other Medical Conditions
High Blood Pressure. High blood pressure (hypertension) contributes to the thickening of the heart’s blood vessel walls, which can worsen atherosclerosis (accumulated deposits of cholesterol in the blood vessels). High blood pressure, high cholesterol, and diabetes all act together to increase the risk for developing heart disease.
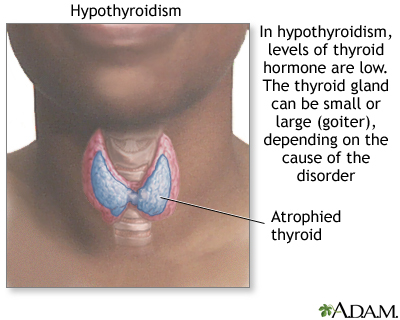
Hypothyroidism. Low thyroid levels (hypothyroidism) are associated with higher total and LDL cholesterol and triglyceride levels. Treating the thyroid condition can significantly reduce cholesterol levels. Research is mixed on whether mild hypothyroidism (subclinical hypothyroidism) is associated with unhealthy cholesterol levels.
Polycystic Ovarian Syndrome. Women with this endocrine disorder may have increased risks for high triglyceride and low HDL levels. This risk may be due to the higher levels of the male hormone testosterone associated with this disease.
Kidney Disease. Kidney disease increases the risk of heart disease.
Other Risk Factors
Medications. Certain medications such as specific antiseizure drugs, corticosteroids, and isotretinoin (Accutane) may increase lipid levels.
Complications
Heart Disease
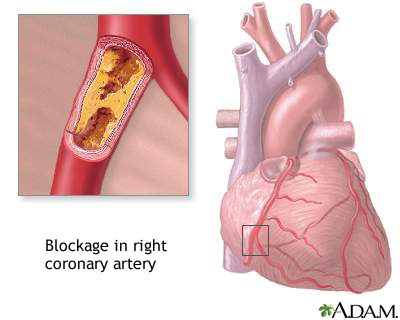
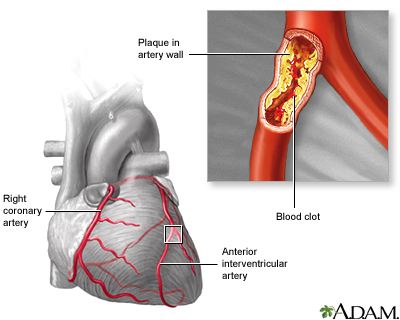
Unhealthy cholesterol, particularly low-density lipoprotein (LDL) cholesterol, forms a fatty substance called plaque, which builds up on the arterial walls of the heart. Smaller plaques remain soft, but older, larger plaques tend to develop fibrous caps with calcium deposits.
The long-term result is atherosclerosis, commonly called hardening of the arteries. The heart is endangered in two ways by this process:
- Eventually these calcified and inelastic arteries become narrower (a condition known as stenosis). As this process continues, blood flow slows and prevents sufficient oxygen-rich blood from reaching the heart. This condition leads to angina (chest pain) and, in severe cases, to heart attack.
- Smaller unstable plaques may rupture, triggering the formation blood clots on their surface. The blood clots block the arteries and are important causes of heart attack.
This process is accelerated by other risk factors including high blood pressure, smoking, obesity, diabetes, and a sedentary lifestyle. When more than one of these risk factors is present, the risk is compounded.
Coronary Artery Disease. The end result of atherosclerosis is coronary artery diseas. Coronary artery disease, commonly known as heart disease, is the leading cause of death in the U.S.
Studies consistently report a higher risk for death from heart disease with high total cholesterol levels (200 mg/dL and higher). The higher the cholesterol, the greater the risk. On average, every time a person's total cholesterol level drops by a point, the risk of heart disease drops by 2%.
Peripheral Artery Disease
Peripheral artery disease (PAD) is caused by the buildup of plaque in the feet, legs, hands, and arms. It most often occurs in the legs. PAD is associated with atherosclerosis. The risk for PAD increases by 5 - 10% with every 10 mg/dL increase in total cholesterol levels. Lower levels of HDL and high triglyceride levels also increase the risk for PAD.
Stroke
Having adequate levels of HDL may be the most important lipid-related factor for preventing ischemic stroke, a type of stroke caused by blockage of the arteries that carry blood to the brain. HDL may even reduce the risk for hemorrhagic stroke, a much less common type of stroke caused by bleeding in the brain that is associated with low overall cholesterol levels.
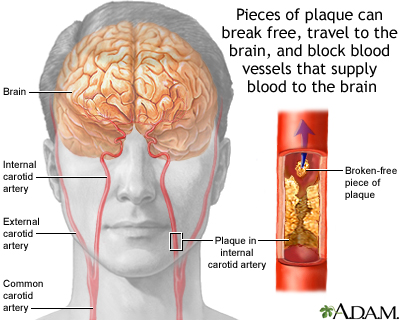
The effects of high total cholesterol and LDL levels on ischemic stroke are less clear. Some research suggests that the risk for ischemic stroke increases when total cholesterol is high. Other studies suggest that high cholesterol poses a risk for stroke only when specific proteins associated with inflammation are present.
Symptoms
There are no warning signs for high LDL and other unhealthy cholesterol levels. When symptoms finally occur, they usually take the form of angina (chest pain) or heart attack in response to the buildup of atherosclerotic plaque in the heart arteries.
Diagnosis
Blood tests can easily measure cholesterol levels. A blood test for cholesterol should include the entire lipoprotein profile: LDL, total cholesterol, HDL, and triglycerides. It is very difficult to measure LDL levels by themselves, but LDL levels can be reliably calculated using total cholesterol and HDL levels.
To obtain a reliable cholesterol reading, doctors advise:
- Do not eat or drink anything but water for 12 hours before the test.
- If the test results are abnormal, a second test should be performed between 1 week and 2 months after the first test.
Screening Guidelines
Periodic cholesterol testing is recommended in all adults, but the major national guidelines differ on the age to start testing.
- Recommended starting ages are between 20 - 35 for men and 20 - 45 for women.
- Adults with normal cholesterol levels do not need to have the test repeated for 5 years unless changes occur in lifestyle (including weight gain and diet).
- Adults with a history of elevated cholesterol, diabetes, kidney problems, heart disease, and other conditions require more frequent testing.
Screening with a fasting lipid profile is recommended for children who:
- Have risk factors such as a family history of high cholesterol, and history of heart attacks before age 55 for men and before age 65 for women. Screening should begin as early as age 2 and no later than age 10.
- Are obese (above 85th percentile for weight) or who have diabetes. If the child’s cholesterol level tests normal, retesting is recommended in 3 - 5 years.
Patients already being treated for high cholesterol should be checked every 2 - 6 months.
Treatment
Lifestyle changes (such as diet, weight control, exercise, and smoking cessation) are the first line of defense for treating unhealthy cholesterol levels. If levels still remain high, drug treatment is an effective next step. Statins are the first-line drugs for reducing high LDL levels. However, while statins have been shown to slow the rate of atherosclerotic progression, they have not yet been shown to reverse heart disease.
Reducing LDL (“bad” cholesterol) and total cholesterol levels, while at the same time boosting HDL (“good” cholesterol) levels, can prevent heart attacks and death in all people (with or without heart disease). Reducing LDL is the primary goal of most cholesterol drugs. (Some medications aim to increase HDL levels, but it is still unclear whether raising HDL levels without lowering LDL levels helps prevent heart disease.) Cholesterol-lowering medications are used along with healthy lifestyle habits, not in place of them. Lowering cholesterol levels with lifestyle changes and drug treatment has been shown to decrease the risk of heart attacks and other complications of atherosclerosis.
The National Cholesterol Education Program’s (NCEP) clinical practice guidelines set treatment goals for LDL levels based on a patient's risk factors for heart disease. The risk factors include:
- Having a first-degree female relative diagnosed with heart disease before age 65 or a first-degree male relative diagnosed before age 55
- Being male and over age 45 or female and over age 55
- Cigarette smoking
- Diabetes
- High blood pressure
- Metabolic syndrome (risk factors associated with obesity such as low HDL levels and high triglycerides)
Two or more of these risk factors increases by 20% the chance of having a heart attack within 10 years.
The LDL cholesterol level is one of the most important factors in determining whether a patient needs cholesterol therapy and whether the treatment is working properly. In particular, guidelines emphasize lower LDL levels and earlier treatment for people with coronary artery disease, or other forms of atherosclerosis, and diabetes. (For a table of Cholesterol Goals for Adults, see Introduction section of this report.)
Although current cholesterol goals are extremely useful for most patients, sometimes results of the testing are difficult to interpret and make it difficult for doctors to decide on the appropriate treatment. This is especially true for patients whose test results show:
- Low LDL levels (which are protective) but also low HDL or high triglycerides (which are harmful)
- High total cholesterol levels (which are harmful) but also high HDL levels (which are protective)
Starting Medications. Even modest lowering of high cholesterol levels, whether through drug therapy or lifestyle changes, reduces the risk of disability and death from heart disease. Most drug treatment now focuses on lowering LDL ("bad") cholesterol. A doctor will start or consider medication, increase dosage of medication, or add new medication when a patient’s:
- LDL cholesterol is 190 mg/dL or higher.
- LDL cholesterol is 160 mg/dL or higher AND patient has one risk factor for heart disease.
- LDL cholesterol is 130 mg/dL or higher AND patient has either diabetes or two other risk factors for heart disease.
- LDL cholesterol is 100 mg/dL or higher AND patient has heart disease. (If patient has diabetes, even without heart disease, medication may be considered for an LDL cholesterol of 100 mg/dL.)
- LDL cholesterol is greater than 70 mg/dL AND patient has had a recent heart attack or has known heart disease along with diabetes, current cigarette smoking, poorly controlled high blood pressure, or the metabolic syndrome (high triglycerides, low HDL, and obesity).
Statins are usually the first type of drug used. Statin therapy has been proven to decrease the risk of heart attack, stroke, and the need for coronary revascularization procedures.
In 2010, the FDA approved the statin drug rosuvastatin (Crestor) for prevention of heart attack and stroke in patients with normal LDL cholesterol levels who have a combination of other risk factors that put them at increased risk for heart disease. Rosuvastatin may now be prescribed as primary prevention for men ages 50 years or older or women ages 60 years or older who have:
- High C-reactive protein levels (2 mg/L or higher) AND
- At least one other cardiovascular risk factor (high blood pressure, low HDL cholesterol, smoking, family history of premature heart disease)
C-reactive protein (CRP) is a protein that helps measure inflammation in the body. Increased CRP levels indicate more inflammation and increased risk for heart disease.
Choosing the Correct Lipid-Lowering Medication. Doctors recommend that drug treatments be individually tailored for raising or lowering specific lipids, depending on the patient's blood lipid picture:
- Statins are the standard drugs for most people who require LDL-lowering therapy.
- If LDL goals are not achieved, combinations of a statin with a bile-acid resin should be considered.
- Fibrates may be beneficial for people who need to lower triglycerides and increase HDL.
Considerations for Children and Adolescents. Lifestyle modifications (diet, exercise) are the first course of action for treating children who have unhealthy cholesterol levels or who are at risk for them. In 2008, the American Academy of Pediatrics (AAP) recommended prescribing statin drugs for children age 8 and older who have elevated LDL levels of 190 mg/dLor over. The AAP also recommended statins for children with LDL 160 mg/dL if there is a family history of heart disease or other risk factors.
For children with diabetes, cholesterol drug treatment is recommended when LDL levels are 130 mg/dL. The goal is to lower LDL levels to less than 160 mg/dL or even 110 mg/dL for children with strong risk factors. However, the issue of prescribing statins to children is being hotly debated within the medical community.
Considerations for People with Diabetes. At this time, statins are recommended as the best drugs for improving cholesterol and lipid levels in people with diabetes. However, recent evidence suggests that statin drugs, especially when given in high doses, may increase blood sugar levels. Still, studies indicate that statins can reduce the risk for adverse heart events, even if patients' cholesterol levels are normal or if their diabetes is mild. Fibrates may also be useful for some people with type 2 diabetes although it is unclear how much benefit they have.
Medications
Statins
Statins are considered the most effective drugs for the treatment of high cholesterol in most patients, particularly for lowering LDL levels. They also have modest effects in lowering triglycerides and increasing HDL levels. Statins inhibit the liver enzyme HMG-CoA reductase, which the body uses to manufacturer of cholesterol. These drugs effectively reduce the risk of major coronary events, including first and second heart attacks and stroke, in adults with unhealthy cholesterol levels.
Current guidelines from the American College of Cardiology and American Heart Association recommend a statin drug as the first-line treatment for patients with atherosclerosis whose LDL levels are higher than 100 mg/dL.
Brands. Statins approved in the U.S. include:
- Lovastatin (Mevacor, generic)
- Pravastatin (Pravachol, generic)
- Simvastatin (Zocor, generic)
- Atorvastatin (Lipitor, generic)
- Fluvastatin (Lescol)
- Pitavastatin (Livalo)
- Rosuvastatin (Crestor)
Statins may also be prescribed as fixed-dose combination drugs, which combine two drugs in one pill:
- Ezetimibe/simvastatin (Vytorin) combines two cholesterol medications that work in different ways.
- Amlodipine/atorvastatin (Caduet) is a dual-therapy medication that combines the antihypertensive calcium channel blocker amlodipine with atorvastatin. It is used to treat simultaneously high blood pressure and high cholesterol.
- Sitagliptin/simvastatin (Juvisync) combines the diabetes drug sitagliptin (Januvia) with simvastatin. It is used to treat simultaneously type 2 diabetes and high cholesterol.
Statins may be prescribed along with other cholesterol-lowering drugs, such as bile acid-binding resins and fibrates.
Side Effects. Statins tend to be better tolerated than other cholesterol-lowering drugs. Side effects may include gastrointestinal discomfort, headaches, skin rashes, muscle aches, sexual dysfunction, drowsiness, dizziness, nausea, constipation, and peripheral neuropathy (numbness or tingling in the hands and feet).
In general, a statin drug should be started at a lower dose and raised incrementally until healthy cholesterol levels are maintained. Patients should immediately tell their doctor about any unusual muscle discomfort or weakness, fever, nausea or vomiting, or darkening of urine color.
A specific safety concern with statins is an uncommon condition called myopathy, in which a patient may experience muscle pains and certain lab tests may be elevated. A myopathy called rhabdomyolysis can lead to kidney failure, but fortunately its occurrence is very rare. The risk for myopathy/rhabdomyolysis is highest at higher doses and in older people (over 65 years), those with hyperthyroidism, and those with renal insufficiency (kidney disease). Both statins and fibrates carry a risk for myopathy. The combination of the two drugs increases this side effect. Some people who use a statin-fibrate combination withdraw from the regimen because of muscle discomfort.
Rosuvastatin (Crestor) may in particular increase the risk for myopathy, especially when given at the highest dose level (40 mg). The FDA advises that patients should not start therapy at a high dose. In addition, people of Asian heritage appear to metabolize the drug differently and should start treatment at the lowest rosuvastatin dose (5 mg). Maximal doses of simvastatin also appear to increase the risk of myopathy.
Statins can also affect the liver, particularly at higher doses. Liver enzyme tests should be performed before starting statin therapy. Patients should notify their doctors if they have symptoms that indicate liver problems such as unusual fatigue, loss of appetite, upper belly pain, dark-colored urine or yellowing of the skin or whites of the eyes. Extra care is recommended for patients who have liver disease. Women who are pregnant or breastfeeding should not use statins. High doses of statins may increase the risk for kidney failure, particularly for patients with other existing risk factors (such as diabetes, hypertension, atherosclerosis, and a history of heart failure).
In 2012, the FDA updated the labels of statin drugs to include additional safety information. The updated labels note that statins have been associated with certain cognitive (mental) effects including memory loss and confusion. These symptoms cease once the statin medication is stopped. Another new safety concern pertains to increases in blood sugar levels (hyperglycemia). Patients being treated with statins may have a small increased risk of hyperglycemia and of being diagnosed with type 2 diabetes.
Interactions with Drugs and Food. Statins may have some adverse interactions with other drugs, including other cholesterol-lowering medications. Patients should tell their doctors about any other medications they are taking. Medications that should never be taken along with statins include protease inhibitors, telaprevir, cyclosporine, macrolide antibiotics, and certain antifungals. Grapefruit juice and Seville oranges can increase the blood levels of certain statins.
Niacin (nicotinic acid)
For many years, high doses of niacin (vitamin B3) were considered a treatment option for low HDL cholesterol and high LDL cholesterol and triglyceride levels. However, in 2011, the National Institutes of Health halted a clinical trial on adding high-dose niacin to statin treatment. The researchers found that while this drug combination did raise HDL levels, it did not reduce the risk of cardiovascular events, including heart attacks and stroke, any more than the statin alone .
Fibrates
Brands. Fibrates (sometimes called fibric acid derivatives) break down the particles that make triglycerides. Gemfibrozil (Lopid, generic) is the standard fibrate. It is usually taken twice a day, 30 minutes before breakfast and before the evening meal. Other fibrates include fenofibrate (Tricor, Lofibra) and fenofibric acid (Trilipix).
Benefits. Fibrates have the following effects on cholesterol, lipids, and other factors:
- They may be good choices for patients who need to lower triglyceride levels and increase HDL but who cannot take other drugs used for these purposes, such as nicotinic acid.
- Fibrates can produce modest reductions in LDL levels, although not as effectively as statins or other drugs. LDL may actually increase in patients with very high triglycerides who take these drugs.
- Recent studies have questioned fibrates’ usefulness in cholesterol treatment. The FDA warns that fenofibric acid may not lower a patient’s risk of having a heart attack or stroke. Other studies advise that high-risk patients with diabetes may not benefit from fenofibrate as it does little to affect heart outcomes and can worsen kidney function.
Side Effects. Side effects may include gastrointestinal discomfort, aching muscles, sensitivity to sunlight, and skin rashes. Fibrates have been known to cause gallstones, so people with gallbladder problems should not use these drugs.
The drugs may cause abnormal heart rhythms and can affect the liver and kidney.
Drug Interactions. Fibrates interact with a number of drugs and substances, including warfarin, some oral drugs used for diabetes, certain antibiotics, and grapefruit juice.
Bile-Acid Binding Resins
Bile-acid binding resins work, as their name suggests, by binding to bile in the digestive tract. This reduces cholesterol in the following way:
- Bile is made in the liver and is used as one of the body's primary manufacturing components.
- Once the resins bind to bile in the digestive tract, the bile is excreted in feces.
- As the resins eliminate bile from the body, the liver takes more cholesterol from the bloodstream in order to produce more bile.
- As cholesterol is taken out of the bloodstream, LDL levels drop.
Brands. Cholestyramine (Questran, Questran Light, generic) is commonly used in a powder that is dissolved in liquid. Colesevelam (Welchol) is available in tablet form. Colestipol (Colestid, generic) is another type of resin drug.
Side Effects. None of these drugs poses major risks. Most, however, cause constipation, heartburn, gas, and other gastrointestinal problems, side effects that many people cannot tolerate. Colesevelam, a newer resin, appears to have significantly fewer of these side effects.
Bile-acting drugs may contribute to calcium loss and therefore increase the risk for osteoporosis. Over time, deficiencies of vitamins A, D, E, and K may occur, and vitamin supplements may be necessary.
Bile acid binders can also elevate triglyceride levels. Rarely, toxic effects on the liver have been reported. Patients with liver disorders should be monitored.
Bile-acid binding resins may also interfere with the absorption of other medications, including digoxin, thyroid replacement hormones, warfarin, beta-blocker drugs, and a number of medications used to treat low blood sugar. In order to prevent drug interactions, other drugs should be taken one hour before or 4 - 6 hours after taking the bile acid-binding resins.
Ezetimibe
Ezetimibe (Zetia) blocks absorption of cholesterol that comes from food. Ezetimibe is usually prescribed in combination with other cholesterol-lowering drugs, when diet and the other drug alone do not work well enough. Examples are:
- As an add-on drug with a statin drug for high LDL levels. However, in a clinical trial the combination of ezetimebe and a statin was no more beneficial than the statin alone.
- In combination with fenofibrate (Tricor) for patients with mixed hyperlipidemia (high LDL levels, high triglycerides, low HDL levels).
The exact role and place for using ezitimbe versus other lipid-lowering drugs for the reduction of risk for heart disease or stroke is not clear.
Vytorin, is a combination of ezetimbe and the statin simvastatin in a single pill. This combination pill should not be used along with fibrate drugs.
Lovaza
Lovaza is a prescription form of omega-3 fish oil, which may be prescribed to help lower triglyceride levels. Side effects include burping and a fishy taste. LDL levels may increase in some patients.
Lifestyle Changes
The absolute mandate for improving cholesterol levels is to first make changes in lifestyle (both diet and exercise). Even when drugs are used, healthy diet and physical activity are critical companions.
Heart-Healthy Diets
There are many major dietary approaches for protecting health, such as the Mediterranean diet, which emphasizes fruits, vegetables, and healthy types of fats. Doctors generally agree on the following recommendations for heart protection:
- Choose fiber-rich food (whole grains, legumes, and nuts) as the main source of carbohydrates, along with a high intake of fruits and vegetables. Walnuts in particular have cholesterol-lowering properties and are a good source of antioxidants and alpha-linolenic acid.
- Avoid saturated fats (found mostly in animal products and tropical plant oils) and trans fatty acids (found in hydrogenated fats and many commercial products and fast foods). Choose unsaturated fats (particularly omega-3 fatty acids found in vegetable [olive, canola] and fish oils). For dairy products, choose non fat or low fat over whole fat.
- Avoid added sugars such as those found in sugar-sweetened beverages.
- For proteins, choose fish, poultry, and beans instead of red meat.
- Fish is particularly heart protective. People who don't or won't eat fish can take a daily fish oil supplement. Omega-3 fatty acid fish oil supplements contain docasahexaenoic (DHA) and eicosapentaenoic (EPA) acids, which have significant benefits for the heart, particularly for lowering triglyceride levels. Fish oil supplements are also available in prescription form (Lovaza).
- Controlling weight, quitting smoking, and exercising are essential companions of any diet program. In particular, triglyceride levels are closely linked to weight: a 5 - 10% weight loss can result in a 20% decrease in triglyceride measurements.
After embarking on any heart healthy diet, it generally takes an average of 3 - 6 months before any noticeable reduction in cholesterol occurs. However, some people see improved levels in as few as 4 weeks. An intensive program may be necessary to achieve significant improvements in cholesterol levels and to reduce heart risk factors.
Exercise
Inactivity is one of the four major risk factors for coronary artery disease, on par with smoking, unhealthy cholesterol, and high blood pressure. In fact, studies suggest that people who change their diet in order to control cholesterol only achieve a lower risk for heart disease when they also follow a regular aerobic exercise program. Resistance (weight) training offers a complementary benefit to aerobics.
Even moderate exercise reduces the risk of heart attack and stroke. Current guidelines recommend at least 30 minutes of moderate-intensity physical activity on five or more days per week for a total of at least 150 minutes per week.
Quitting Smoking
Cigarette smoking lowers HDL and is directly responsible for about 20% of all deaths from heart disease. The importance of breaking this habit cannot be emphasized enough. Once a person quits smoking, HDL cholesterol levels rise within weeks or months to levels that are equal to their nonsmoking peers. Passive smoking also reduces HDL levels and increases the risk of heart disease in people exposed to second-hand smoke. Cigarette smoking is also associated with high blood pressure.
Alcohol
A number of studies have found heart protection from moderate intake of alcohol (one or two glasses a day). Moderate amounts of alcohol help raise HDL levels. Although red wine is most often cited for healthful properties, any type of alcoholic beverage appears to have similar benefit. People with high triglyceride levels should drink sparingly, or not at all, because even small amounts of alcohol can significantly increase blood triglycerides. Pregnant women, anyone who cannot drink moderately, and people with liver disease should not drink at all.
Herbs and Supplements
Manufacturers of herbal remedies and dietary supplements do not need FDA approval to sell their products. Just like a drug, herbs and supplements can affect the body's chemistry, and therefore have the potential to produce side effects that may be harmful. There have been a number of reported cases of serious and even lethal side effects from herbal products. Always check with your doctor before using any herbal remedies or dietary supplements.
The following natural remedies are of interest for cholesterol control:
- Garlic. Contrary to popular belief, neither raw garlic nor garlic supplements significantly reduce LDL cholesterol levels.
- Policosonol. Policosanol is a nutritional supplement derived from sugar cane that has been promoted as having lipid-lowering benefits. However, rigorous research has not shown that policosanol has any effect on reducing LDL levels.
- Red Yeast Rice. Red yeast rice is used in traditional Chinese medicine. The FDA warns that red yeast rice dietary supplement products sold as treatments for high cholesterol contain the same chemicals as the statin drugs, but these products are not standardized for purity, safety, and effectiveness.
Resources
- www.nhlbi.nih.gov/about/ncep -- National Cholesterol Education Program
- www.nhlbi.nih.gov -- National Heart, Lung, and Blood Institute
- www.acc.org -- American College of Cardiology
- www.heart.org-- American Heart Association
- www.eatright.org -- American Dietetic Association
References
ACCORD Study Group, Ginsberg HN, Elam MB, Lovato LC, Crouse JR 3rd, Leiter LA, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010 Apr 29;362(17):1563-74. Epub 2010 Mar 14.
AIM-HIGH Investigators, Boden WE, Probstfield JL, Anderson T, Chaitman BR,Desvignes-Nickens P, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011 Dec 15;365(24):2255-67. Epub 2011 Nov 15.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009 Oct 20;120(16):1640-5. Epub 2009 Oct
Armitage J. The safety of statins in clinical practice. Lancet. 2007 Nov 24;370(9601):1781-90.
Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, et al. HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med. 2007 Sep 27;357(13):1301-10.
Briel M, Ferreira-Gonzalez I, You JJ, Karanicolas PJ, Akl EA, Wu P, et al. Association between change in high density lipoprotein cholesterol and cardiovascular disease morbidity and mortality: systematic review and meta-regression analysis. BMJ. 2009 Feb 16;338:b92. doi: 10.1136/bmj.b92.
Cholesterol Treatment Trialists’ (CTT) Collaboration, Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010 Nov 13;376(9753):1670-81. Epub 2010 Nov 8.
Crouse JR 3rd, Raichlen JS, Riley WA, Evans GW, Palmer MK, O'Leary DH, et al. Effect of rosuvastatin on progression of carotid intima-media thickness in low-risk individuals with subclinical atherosclerosis: The METEOR Trial. JAMA. 2007 Mar 25; [Epub ahead of print]
Daniels SR, Greer FR; Committee on Nutrition. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008 Jul;122(1):198-208.
Drozda J Jr, Messer JV, Spertus J, Abramowitz B, Alexander K, Beam CT, et al. ACCF/AHA/AMA-PCPI 2011 performance measures for adults with coronary artery disease and hypertension: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement. J Am Coll Cardiol. 2011 Jul 12;58(3):316-36. Epub 2011 Jun 14.
Gaziano M, Ridker PM, Libby P. Primary and secondary prevention of coronary heart disease. In: Bonow RO, Mann DL, Zipes DP, Libby P, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Saunders; 2012:chap 49.
Hlatky MA. Expanding the orbit of primary prevention -- moving beyond JUPITER. N Engl J Med. 2008 Nov 20;359(21):2280-2. Epub 2008 Nov 9.
Jackevicius CA, Tu JV, Ross JS, Ko DT, Carreon D, Krumholz HM. Use of fibrates in the United States and Canada. JAMA. 2011 Mar 23;305(12):1217-24.
Kodama S, Tanaka S, Saito K, Shu M, Sone Y, Onitake F, et al. Effect of aerobic exercise training on serum levels of high-density lipoprotein cholesterol: a meta-analysis. Arch Intern Med. 2007 May 28;167(10):999-1008.
Kuklina EV, Yoon PW, Keenan NL. Trends in high levels of low-density lipoprotein cholesterol in the United States, 1999-2006. JAMA. 2009 Nov 18;302(19):2104-10.
McCrindle BW, Urbina EM, Dennison BA, Jacobson MS, Steinberger J, Rocchini AP, et al. Drug therapy of high-risk lipid abnormalities in children and adolescents. A scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee, Council of Cardiovascular Disease in the Young, With the Council on Cardiovascular Nursing. Circulation. 2007 Mar 21; [Epub ahead of print]
Miller M, Stone NJ, Ballantyne C, Bittner V, Criqui MH, Ginsberg HN, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011 May 24;123(20):2292-333. Epub 2011 Apr 18.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010 Sep 28;56(14):1113-32.
Preiss D, Seshasai SR, Welsh P, Murphy SA, Ho JE, Waters DD, et al. Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA. 2011 Jun 22;305(24):2556-64.
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008 Nov 20;359(21):2195-207. Epub 2008 Nov 9.
Sharma M, Ansari MT, Abou-Setta AM, Soares-Weiser K, Ooi TC, Sears M, et al. Systematic review: comparative effectiveness and harms of combination therapy and monotherapy for dyslipidemia. Ann Intern Med. 2009 Nov 3;151(9):622-30.
Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011 Nov 29;58(23):2432-46. Epub 2011 Nov 3..
US Preventive Services Task Force. Screening for lipid disorders in children: US Preventive Services Task Force recommendation statement. Pediatrics. 2007 Jul;120(1):e215-9.
|
Review Date:
5/22/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |






